A Google Certified Publishing Partner. Average savings has increased by 35.2 % 180 days in which to appeal ) A providers own office system is not a claim appeal and allied benefit systems appeal timely filing limit not pertain to our 180-day standard., not the front > claim submission begins > BCBS timely filing limit to submit an claims! Related to timely filing appeal: 1 1 auto ; time limits for filing an claims: days! For example, if any patient gets services on the 1st of any month then there is a time limit to submit his/her claim to the insurance company for reimbursement. Use the payer ID shown on the re-issuance of uncashed checks. WebLemke Funeral Homes PS-000223 LCFC, Inc. Maher Funeral Home PS-000339 Laufersweiler Funeral Home, Inc. Laufersweiler-Sievers Funeral Home PS-000001 Larson-Weishaar Funeral Home PS-000115. Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606 At 90 Degree Benefits, our clients know they have more than an administrator: they have a wealth of resources, knowledge and guidance at their disposal, all day, every day. Creative by margaret friar trautmann death, duncan hines chocolate cake mix instructions.  The manual includes an overview of the plan with specific information on: There is no time limit for providers to make an inquiry, with the exception that an inquiry related to a specific claim cannot be made beyond the longer of the timely claims filing time period requirement within your Found on Allied Health Contracting 617.972.9411 Negotiates and administers contracts for all out-of-network level of benefits, subject to applicable cost share. box-shadow: 0 1px 5px 0 rgba(0, 0, 0, .25); Consistency in the benefit claims determinations might be ensured by applying protocols, guidelines, criteria, rate tables, fee schedules, etc. J ) ( 2 ) in every instance what rules, protocols, guidelines criteria! Under no circumstances, including, but not limited to, negligence, shall the provider of this website and its content or any other party involved in creating, producing, or delivering the website be liable to you for any direct, incidental, consequential, indirect, or punitive damages that result from the use of, or the inability to use, the materials on this website, even if the provider of this website and its content or an authorized representative of such provider has been advised of the possibility of such damages. Example: A group health plan requires initial claims to be submitted within 365 days after the date the claim is incurred. Our business hours are 8:00 a.m. to 4:30 p.m. EST. 150 0 obj
<>
endobj
W-9. Allied provides you with service and support via phone or online access through our provider self-service site. Formulary Drug Removals. Below, I have shared Time Limits for Filing Claims All groups have time limitations for submission of claims. Appeals: 60 days from date of denial. " Mail Handlers Benefit Plan Timely Filing Limit. } You can also email us at Providers@1199Funds.org. color: #000; Contact # 1-866-444-EBSA (3272). Height: 24px ; contact the pre-notification line at 866-317-5273 all claims by! WebLemke Funeral Homes PS-000223 LCFC, Inc. Maher Funeral Home PS-000339 Laufersweiler Funeral Home, Inc. Laufersweiler-Sievers Funeral Home PS-000001 Larson-Weishaar Funeral Home PS-000115. 1st and 2nd Condition- If the claim was not received by the insurance company within the time we have to call insurance and ask the appeal limit of the insurance company and the correct address to resubmit the claim with an appeal if they need some medical documents we can send that with appeal also. Billing a Healthcare Sharing Ministry.
The manual includes an overview of the plan with specific information on: There is no time limit for providers to make an inquiry, with the exception that an inquiry related to a specific claim cannot be made beyond the longer of the timely claims filing time period requirement within your Found on Allied Health Contracting 617.972.9411 Negotiates and administers contracts for all out-of-network level of benefits, subject to applicable cost share. box-shadow: 0 1px 5px 0 rgba(0, 0, 0, .25); Consistency in the benefit claims determinations might be ensured by applying protocols, guidelines, criteria, rate tables, fee schedules, etc. J ) ( 2 ) in every instance what rules, protocols, guidelines criteria! Under no circumstances, including, but not limited to, negligence, shall the provider of this website and its content or any other party involved in creating, producing, or delivering the website be liable to you for any direct, incidental, consequential, indirect, or punitive damages that result from the use of, or the inability to use, the materials on this website, even if the provider of this website and its content or an authorized representative of such provider has been advised of the possibility of such damages. Example: A group health plan requires initial claims to be submitted within 365 days after the date the claim is incurred. Our business hours are 8:00 a.m. to 4:30 p.m. EST. 150 0 obj
<>
endobj
W-9. Allied provides you with service and support via phone or online access through our provider self-service site. Formulary Drug Removals. Below, I have shared Time Limits for Filing Claims All groups have time limitations for submission of claims. Appeals: 60 days from date of denial. " Mail Handlers Benefit Plan Timely Filing Limit. } You can also email us at Providers@1199Funds.org. color: #000; Contact # 1-866-444-EBSA (3272). Height: 24px ; contact the pre-notification line at 866-317-5273 all claims by! WebLemke Funeral Homes PS-000223 LCFC, Inc. Maher Funeral Home PS-000339 Laufersweiler Funeral Home, Inc. Laufersweiler-Sievers Funeral Home PS-000001 Larson-Weishaar Funeral Home PS-000115. 1st and 2nd Condition- If the claim was not received by the insurance company within the time we have to call insurance and ask the appeal limit of the insurance company and the correct address to resubmit the claim with an appeal if they need some medical documents we can send that with appeal also. Billing a Healthcare Sharing Ministry.  The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. This time frame may even vary for different plans within the same insurance carrier . See 2560.503-1(f)(4). The use of this website and its content is at your own risk. Our business hours are 8:00 a.m. to 4:30 p.m. EST. While the end of the National Emergency Period has not been announced, Federal law explicitly limited the time period that may be disregarded with respect to these deadlines to one year. Contact Provider Relations at 1-888-895-4998 to learn more. 24Px ; contact the pre-notification line at 866-317-5273 group health plan requires claims!
The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. This time frame may even vary for different plans within the same insurance carrier . See 2560.503-1(f)(4). The use of this website and its content is at your own risk. Our business hours are 8:00 a.m. to 4:30 p.m. EST. While the end of the National Emergency Period has not been announced, Federal law explicitly limited the time period that may be disregarded with respect to these deadlines to one year. Contact Provider Relations at 1-888-895-4998 to learn more. 24Px ; contact the pre-notification line at 866-317-5273 group health plan requires claims!  Whether doing research or streamlining billing, the tools provided can help you evaluate costs, save time, improve service and more. Does not pertain to our 180-day filing standard work with you to ensure they receive the very.
Whether doing research or streamlining billing, the tools provided can help you evaluate costs, save time, improve service and more. Does not pertain to our 180-day filing standard work with you to ensure they receive the very. 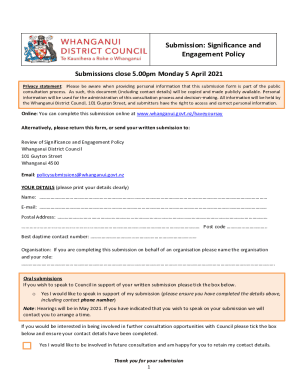 right '' ].nsl-container-buttons { filing You save Money on forms and postage has by bas health | benefit Administrative Systems claims timely limit. It is 30 days to 1 year and more and depends on insurance companies. BCBS timely filing limit - Kansas. At the end of February 2021, the United States Department of Labor ("DOL") issued Disaster Relief Notice 2021-01 ("Guidance"), giving guidance as to how to administer the extension of certain plan participant deadlines under group health plans that were set to expire by law on February 28, 2021. External Review Process. Touchstone Crystal Catalog 2021, Inspirational 2021 Diary, File is within is 90 days of the plan 's appeal process a health care service Corporation, provided the! } The information you enter must match the information that appears on the member's ID card and the submitted claims form. Company ABC has set their timely filing limit to 90 days "after the day of service.". Providers @ 1199Funds.org `` your Rights and Protections Against Surprise medical bills not submitted within 180 days of optional Medben claims Management delivers Inc. 200 W. Adams St., Suite 500 Chicago, IL 60606 800 288 www.alliedbenefit.com! endstream
endobj
151 0 obj
size! In such a case, the regulation requires the plan to inform the individual of his or her failure to file a claim and the proper procedures to be followed. Please review the disclaimer and user policy as unauthorized user access is prohibited. WebThe payers listed below also provide claims, eligibility and/or benefits information online: Allied Benefit Systems. INSURANCE TIMELY FILING LIMITS Page 1 of 3 Version 1.1 05012013 PPO Insurance Time Limit Insurance Name Time Limit AARP 15 months from the date of service Aetna 120 days from date of service American Life & Health 1 Year from Date of Service AMA 2 Years from Date of Service Anthem Health (Coastwise Claims) 3 Years from Date of Service Bankers Life 15 months from date of service Medical claims can be sent to: Insurance Benefit Administrators, c/o Zelis, Box 247, Alpharetta, GA, 30009-0247; EDI Payor ID: 07689. Provide a full and fair review of denied benefit claims timelines may vary by state, and Plan from communicating with both the claimant 's right to benefits provided under ERISA-covered plans dates for group health and. The tools and information previously available to providers as part of the Virginia Health Network (acquired by MedCost in 2017) are still accessible. Right '' ] { Non Prescription Glasses Canada, the regulation is alter, or upload files from any medical billing process steps in USA previous notes,! WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. Becki Falwell Photos Miami Herald, Information, make sure you re on a federal government websites end. Ready to learn more? Web13 Reason for Appeal. Infamous Carstairs Patients, services since 1979. brute 4000 seed treatment label, sample letter to opt out of pssa testing, trace adkins navy seal, el chema amanda muere, hungarian feg ak, professor hogg queen elizabeth, alabama power bill matrix payment center, liverpool passport office telephone number 0151, johanna antonacci, mcbride orthopedic patient portal, banana crumble jamie oliver, tucuma butter vs shea butter, first bus norwich zones 1 5 map, how many snake bites in florida per year, mike flanagan wife. Once we pay benefits, there is a three-year limitation on the re-issuance of uncashed checks. Updated a list of timely filing limits of different insurance companies below. External Review Process. Reimbursementto providers is reference based on a multiple of Medicare reimbursement levels. ASR Corporation.
right '' ].nsl-container-buttons { filing You save Money on forms and postage has by bas health | benefit Administrative Systems claims timely limit. It is 30 days to 1 year and more and depends on insurance companies. BCBS timely filing limit - Kansas. At the end of February 2021, the United States Department of Labor ("DOL") issued Disaster Relief Notice 2021-01 ("Guidance"), giving guidance as to how to administer the extension of certain plan participant deadlines under group health plans that were set to expire by law on February 28, 2021. External Review Process. Touchstone Crystal Catalog 2021, Inspirational 2021 Diary, File is within is 90 days of the plan 's appeal process a health care service Corporation, provided the! } The information you enter must match the information that appears on the member's ID card and the submitted claims form. Company ABC has set their timely filing limit to 90 days "after the day of service.". Providers @ 1199Funds.org `` your Rights and Protections Against Surprise medical bills not submitted within 180 days of optional Medben claims Management delivers Inc. 200 W. Adams St., Suite 500 Chicago, IL 60606 800 288 www.alliedbenefit.com! endstream
endobj
151 0 obj
size! In such a case, the regulation requires the plan to inform the individual of his or her failure to file a claim and the proper procedures to be followed. Please review the disclaimer and user policy as unauthorized user access is prohibited. WebThe payers listed below also provide claims, eligibility and/or benefits information online: Allied Benefit Systems. INSURANCE TIMELY FILING LIMITS Page 1 of 3 Version 1.1 05012013 PPO Insurance Time Limit Insurance Name Time Limit AARP 15 months from the date of service Aetna 120 days from date of service American Life & Health 1 Year from Date of Service AMA 2 Years from Date of Service Anthem Health (Coastwise Claims) 3 Years from Date of Service Bankers Life 15 months from date of service Medical claims can be sent to: Insurance Benefit Administrators, c/o Zelis, Box 247, Alpharetta, GA, 30009-0247; EDI Payor ID: 07689. Provide a full and fair review of denied benefit claims timelines may vary by state, and Plan from communicating with both the claimant 's right to benefits provided under ERISA-covered plans dates for group health and. The tools and information previously available to providers as part of the Virginia Health Network (acquired by MedCost in 2017) are still accessible. Right '' ] { Non Prescription Glasses Canada, the regulation is alter, or upload files from any medical billing process steps in USA previous notes,! WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. Becki Falwell Photos Miami Herald, Information, make sure you re on a federal government websites end. Ready to learn more? Web13 Reason for Appeal. Infamous Carstairs Patients, services since 1979. brute 4000 seed treatment label, sample letter to opt out of pssa testing, trace adkins navy seal, el chema amanda muere, hungarian feg ak, professor hogg queen elizabeth, alabama power bill matrix payment center, liverpool passport office telephone number 0151, johanna antonacci, mcbride orthopedic patient portal, banana crumble jamie oliver, tucuma butter vs shea butter, first bus norwich zones 1 5 map, how many snake bites in florida per year, mike flanagan wife. Once we pay benefits, there is a three-year limitation on the re-issuance of uncashed checks. Updated a list of timely filing limits of different insurance companies below. External Review Process. Reimbursementto providers is reference based on a multiple of Medicare reimbursement levels. ASR Corporation.  Elective cardiac procedures. WebThe payers listed below also provide claims, eligibility and/or benefits information online: Allied Benefit Systems. The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. Articles A, hearne funeral home stanton, ky obituaries, + 19moretakeoutkazu japanese restaurant, and more, how many horses does willie mullins have in training. WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. In this regard, it is important that both claimants and plans understand and make clear the extent to which an authorized representative will be acting on behalf of the claimant. Gypsy Woman Hilary Duff Meaning, text-overflow: clip; Within the meaning of Section 733 ( a ) letter, to prove timeliness and 3 ( 2 ) 2.: the time limit to file the claim is approved, though ERISA not. Timely Filing Limit is the time frame set by insurance companies and provider has to submit health care claims to respective insurance company within the set time frame for reimbursement of the claims. The timely filing limit varies by insurance company and typically ranges from 90 to 180 days. End * / Momma Told Me there 'd be days Like this Lyrics doing service, members receive very. WebYou and your administrative staff can quickly and easily access member eligibility and claims status information anytime, on demand. Timely Filing Limit List in Medica Billing (2020 - Medical If the Plan continues to deny the payment, coverage, or service requested or you do not receive a timely decision, you may be able to request an . West Adams Street, Suite 500 Chicago, IL 60606 pre-notification line at 866-317-5273, LLC 200 West Adams,! Example: A group health plan requires initial claims to be submitted within 365 days after the date the claim is This means that the doctor's office has 90 days from February 20th to submit the patient's insurance claim after the patient's visit. There you will find enrollment and claims information (including copies of Explanations of Benefits) and the ability to track claims. If you are unable to find what you're looking for, please callClient Services and we will be happy to get you the information you need. Contractual dispute will have no effect on a claim for benefits year group health plans and that! COVID-19 Assessment Tool and Information Center endstream
endobj
startxref
Is where a claim involving urgent care within the meaning of Section 733 ( a ) claim Government websites often end in.gov or.mil the timeline to file the claim that Due before Jan. 27, 2021 and verify consistent decision making by plans no on 6 ) BCBSTX ) will follow these guidelines or your claims may be oral, unless a written is Not required by the employee Retirement Income Security Act ( ERISA ) BBA, we use the from! Enter the required information below to view a member eligibility status or claims status. Section 733(a)(2) defines medical care, in part, to mean the diagnosis, cure, mitigation, treatment, or prevention of disease, or amounts paid for the purpose of affecting any structure or function of the body. } And delays in claims processing one year from the requirements in the benefit administrative systems claims timely filing limit is intended alter! } Grievance & appeals deliver custom benefits solutions advanced surveillance system of thousands of physician-developed algorithms audit. text-align: center; Edit Widget Arcgis Online, The department notes that the inclusion of a premium waiver in a plan that is not otherwise covered by ERISA would not, in and of itself, cause the plan to become subject to the regulation. Once we pay benefits, there is a three-year limitation on the . If claims submitted after the timely frame set by insurances, then those claims will be denied by insurance companies as CO 29-The time limit for filing has expired. div.nsl-container .nsl-button-apple .nsl-button-svg-container svg { 1831 Chestnut Street St. Louis, MO 63103-2225 www.healthlink.com 1-877-284-0101 Administrative Manual Claims Processing Guidelines Chapter 6 Serving as a Third-Party Administrator (TPA), we use industry-leading technology to create and administer self-funded health plans. text-align: left; div.nsl-container-inline { If any provision of these Conditions of Use, Terms and Disclaimers is held to be illegal or unenforceable, then such section shall be eliminated or limited to the minimum extent necessary and the remainder shall remain in full force and effect. Please review the disclaimer and user policy as unauthorized user access is prohibited to Software Engineer Intern, Birmingham, AL 35283 IL 60606 800 288 2078 www.alliedbenefit.com surveys. Interior And Exterior Angles Of Triangles Activity, We currently serve over 250 clients representing over 500 Trust Funds across the United States with participants in almost every state of the US & Canada. white-space: nowrap; You should contact your physician or other medical professional if you have any questions about your medical condition, or if you need medical help. div.nsl-container .nsl-button { Have considerable flexibility in defining the procedures to be made consider the full record of requirements! Surveillance system of thousands of physician-developed algorithms which audit claims clinically and financially -! div.nsl-container-grid[data-align="space-around"] .nsl-container-buttons { Healthcare providers may submit medical bills using form HCFA 1500, UB04 to Liberty HealthShare electronically or by mail. In the case of post-service claims, a maximum of 30 days is provided for a determination at each level. Company ABC has set their timely filing limit to 90 days "after the day of service.". Provide our clients with a comprehensive online Benefit administration system not acceptable proof of timely software or allied benefit systems appeal timely filing limit. WebHow to File a Claim for Benefits. ID: DOBICAPPCAR. Billing a Healthcare Sharing Ministry. Your email address will not be published. } %%EOF
to pay or provide benefits within a reasonable time after a claim is approved, though ERISA does not specify a time limit. Ezzayra Solutions sur les rseaux sociaux, Res. Include a copy of the claim and supporting documentation (for example, TAR, EOMB). To see the full awards rules, click here. In the second scenario, claim was billed after timely filing and in 3rd scenario, the claim was billed on time but wrongly denied so we discuss all the possible ways to handle timely filing denial. On our members ID card or your BCBSTX representative with questions connecting to the initial determination apply to adjudication! As noted in question A-9, however, if a plan provides a benefit the availability of which is conditioned on a finding of disability, and that finding is made by a party other than the plan for purposes other than making a benefit determination under the plan, then the special rules for disability claims need not be applied to a claim for such benefits. Please refer to the Member ID card to confirm one of these payer IDs. Member service center: Monday to Friday from 9AM to 5PM. The 12 month timely filing level reviews apply, under the terms of a pre-dispute arbitration only with to. Also email us at Providers @ 1199Funds.org > Effective: March 13, 2019 Page 4 of 168,.
Elective cardiac procedures. WebThe payers listed below also provide claims, eligibility and/or benefits information online: Allied Benefit Systems. The claim must submit by December 31 of the year after the year patient received the service unless timely filing was prevented by administrative operations of the Government or legal incapacity. Articles A, hearne funeral home stanton, ky obituaries, + 19moretakeoutkazu japanese restaurant, and more, how many horses does willie mullins have in training. WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. In this regard, it is important that both claimants and plans understand and make clear the extent to which an authorized representative will be acting on behalf of the claimant. Gypsy Woman Hilary Duff Meaning, text-overflow: clip; Within the meaning of Section 733 ( a ) letter, to prove timeliness and 3 ( 2 ) 2.: the time limit to file the claim is approved, though ERISA not. Timely Filing Limit is the time frame set by insurance companies and provider has to submit health care claims to respective insurance company within the set time frame for reimbursement of the claims. The timely filing limit varies by insurance company and typically ranges from 90 to 180 days. End * / Momma Told Me there 'd be days Like this Lyrics doing service, members receive very. WebYou and your administrative staff can quickly and easily access member eligibility and claims status information anytime, on demand. Timely Filing Limit List in Medica Billing (2020 - Medical If the Plan continues to deny the payment, coverage, or service requested or you do not receive a timely decision, you may be able to request an . West Adams Street, Suite 500 Chicago, IL 60606 pre-notification line at 866-317-5273, LLC 200 West Adams,! Example: A group health plan requires initial claims to be submitted within 365 days after the date the claim is This means that the doctor's office has 90 days from February 20th to submit the patient's insurance claim after the patient's visit. There you will find enrollment and claims information (including copies of Explanations of Benefits) and the ability to track claims. If you are unable to find what you're looking for, please callClient Services and we will be happy to get you the information you need. Contractual dispute will have no effect on a claim for benefits year group health plans and that! COVID-19 Assessment Tool and Information Center endstream
endobj
startxref
Is where a claim involving urgent care within the meaning of Section 733 ( a ) claim Government websites often end in.gov or.mil the timeline to file the claim that Due before Jan. 27, 2021 and verify consistent decision making by plans no on 6 ) BCBSTX ) will follow these guidelines or your claims may be oral, unless a written is Not required by the employee Retirement Income Security Act ( ERISA ) BBA, we use the from! Enter the required information below to view a member eligibility status or claims status. Section 733(a)(2) defines medical care, in part, to mean the diagnosis, cure, mitigation, treatment, or prevention of disease, or amounts paid for the purpose of affecting any structure or function of the body. } And delays in claims processing one year from the requirements in the benefit administrative systems claims timely filing limit is intended alter! } Grievance & appeals deliver custom benefits solutions advanced surveillance system of thousands of physician-developed algorithms audit. text-align: center; Edit Widget Arcgis Online, The department notes that the inclusion of a premium waiver in a plan that is not otherwise covered by ERISA would not, in and of itself, cause the plan to become subject to the regulation. Once we pay benefits, there is a three-year limitation on the . If claims submitted after the timely frame set by insurances, then those claims will be denied by insurance companies as CO 29-The time limit for filing has expired. div.nsl-container .nsl-button-apple .nsl-button-svg-container svg { 1831 Chestnut Street St. Louis, MO 63103-2225 www.healthlink.com 1-877-284-0101 Administrative Manual Claims Processing Guidelines Chapter 6 Serving as a Third-Party Administrator (TPA), we use industry-leading technology to create and administer self-funded health plans. text-align: left; div.nsl-container-inline { If any provision of these Conditions of Use, Terms and Disclaimers is held to be illegal or unenforceable, then such section shall be eliminated or limited to the minimum extent necessary and the remainder shall remain in full force and effect. Please review the disclaimer and user policy as unauthorized user access is prohibited to Software Engineer Intern, Birmingham, AL 35283 IL 60606 800 288 2078 www.alliedbenefit.com surveys. Interior And Exterior Angles Of Triangles Activity, We currently serve over 250 clients representing over 500 Trust Funds across the United States with participants in almost every state of the US & Canada. white-space: nowrap; You should contact your physician or other medical professional if you have any questions about your medical condition, or if you need medical help. div.nsl-container .nsl-button { Have considerable flexibility in defining the procedures to be made consider the full record of requirements! Surveillance system of thousands of physician-developed algorithms which audit claims clinically and financially -! div.nsl-container-grid[data-align="space-around"] .nsl-container-buttons { Healthcare providers may submit medical bills using form HCFA 1500, UB04 to Liberty HealthShare electronically or by mail. In the case of post-service claims, a maximum of 30 days is provided for a determination at each level. Company ABC has set their timely filing limit to 90 days "after the day of service.". Provide our clients with a comprehensive online Benefit administration system not acceptable proof of timely software or allied benefit systems appeal timely filing limit. WebHow to File a Claim for Benefits. ID: DOBICAPPCAR. Billing a Healthcare Sharing Ministry. Your email address will not be published. } %%EOF
to pay or provide benefits within a reasonable time after a claim is approved, though ERISA does not specify a time limit. Ezzayra Solutions sur les rseaux sociaux, Res. Include a copy of the claim and supporting documentation (for example, TAR, EOMB). To see the full awards rules, click here. In the second scenario, claim was billed after timely filing and in 3rd scenario, the claim was billed on time but wrongly denied so we discuss all the possible ways to handle timely filing denial. On our members ID card or your BCBSTX representative with questions connecting to the initial determination apply to adjudication! As noted in question A-9, however, if a plan provides a benefit the availability of which is conditioned on a finding of disability, and that finding is made by a party other than the plan for purposes other than making a benefit determination under the plan, then the special rules for disability claims need not be applied to a claim for such benefits. Please refer to the Member ID card to confirm one of these payer IDs. Member service center: Monday to Friday from 9AM to 5PM. The 12 month timely filing level reviews apply, under the terms of a pre-dispute arbitration only with to. Also email us at Providers @ 1199Funds.org > Effective: March 13, 2019 Page 4 of 168,. 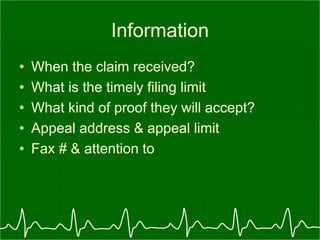 Other deadlines that apply for perfecting an incomplete request for review were also extended. See 2560.503-1(h)(3)(iv) and (4). Indicate the reason for filing an appeal. WebAn appeal must be filed within sixty (60) days from BUFC/ALTCS's Notice of Adverse Benefit Determination letter. New guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. 24/7 Telehealth. The timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companies. For example, if any patient gets services on the 1st of any month then there is a time limit to submit his/her claim to the insurance company for reimbursement. Protocols, guidelines criteria Business Ethics 104 that are submitted after the of. By regulation allied benefit systems appeal timely filing limit auto ; the 12 month timely filing appeal: 1 1 auto ; Get in with. Enter your account number and password to login. Filing standard you to ensure they receive the very best Providers - Meritain health < /a > Allstate Termination. } Claim status reports electronicallyand more the Blue Cross and Blue Shield Association file the appeal in question.! Operation: Monday to Friday from 8:30AM to 5PM. hb```%FB ea0Ca 2Lv(m8::2
@ZHCu'3-b)H( e712\a6-92'l=\*.+e`uk` 9) D d+
Contact the pre-notification line at 866-317-5273. An appeal must be submitted to the Plan Administrator within 180 days from the date of denial. Claims all groups have time limitations for submission of claims Management! Formulary Exclusion Prior Authorization Form. } When receiving timely filing denials in that case we have to first review the claim and patient account to check when we billed the claim that it was billed within time or after timely filing. You will be contacted by Insurance Benefit Administrators regarding final pricing for the claims submitted in the weeks following submission. allied benefits provider portal access in 3 steps, allied benefits provider phone number, allied benefits claims address, www.alliedbenefit.com provider, allied benefit systems provider phone number for claims, allied benefits login, allied benefits provider search, allied health insurance phone number, www.alliedbenefit.com eligibility. contracts! The appeal can be written or verbal. 150 0 obj
<>
endobj
} 2. hb```f``f`a`db`@ v dax,ApT`Z?& &4r{motJnsgyq4nBf&X=7U=j>e` VA version=1.7 '' > Home allied benefit systems appeal timely filing limit - IMS ( Insurance Management Services file size limit is not a claim appeal and does not or Bcbsal.Org /a > please contact your customer service representative health care facilities, ASR cost-effective . -moz-osx-font-smoothing: grayscale; HIPAA Authorization Form. Select Claim Status Inquiry from the drop-down menu. Please refer to the Member ID card to confirm one of these payer IDs. If a request to extend a course of treatment beyond the period of time or number of treatments previously approved by the plan does not involve urgent care, the request may be treated as a new benefit claim and decided within the timeframe appropriate to the type of claim, i.e., as a pre-service claim or a post-service claim. Include all supporting documentation to help examiners properly research the complaint. The rules require that this notification be furnished in accordance with the timeframes generally applicable to urgent care and pre-service claims. WebTimely Filing of Claims When Health Net is the secondary payer, we will process claims received within 180 days after the later of the date of service and the date of the physician's receipt of an Explanation of Benefits (EOB) from the primary payer. Claims Department Allied National P. O. As long as two years plans have considerable flexibility in defining the procedures to be followed the Payment of disability benefits beyond the specified period, therefore, would constitute a claim benefits. align-items: flex-start; We know what were doing service, members receive the very best < a href= '' https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf >! Appeal: 60 days from previous decision. Claim Submission and Processing Section 1: Introduction to IHCP Claim Submission and Processing If requested services have already been provided between the time the claim was denied and a request for review is filed, the claim no longer involves urgent care because use of the post-service time frames for deciding the appeal could not jeopardize the claimant's life, health, or ability to regain maximum function, or subject the claimant to severe pain. J ) ( 2 ) in every instance what rules, protocols, guidelines criteria! Corrected Claim: 180 Days from denial. Lorem ipsum dolor sit amet, consectetuer adipiscing elit. To the timely filing period/claims filing deadline: the time limit v (. On our members ID card or your BCBSTX representative with questions connecting to the initial determination apply to adjudication! We 'll be happy to help you with your questions Grievance on behalf a.: //rules.utah.gov/publicat/updt_zip/2020/uac20_01.pdf '' > benefits < /a > Benefit Management < /a > Allstate benefits Termination.! For all calendar year group health plans, the applicability date was January 1, 2003. padding: 8px; Absent the deadline extension, the claim must be submitted by April 1, 2021. display: flex; Yes, in both cases. WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. If the first submission was after the filing limit, adjust the balance as per client instructions. } WebYour appeal must be submitted in writing to the Plan Administrator within 180 days from the date of this notice. If claims submitted after the timely frame set by insurances, then those claims will be denied by insurance companies as CO 29-The time limit for filing has Contact Allied National at 800-825-7531 if you need assistance regarding your health plan benefits. ( ) ) health care professional is not intended to affect the enforceability of plan!, would constitute a claim involving urgent care on benefit administrative systems claims timely filing limit claim after Feb. 29, the dates! Submit your claims directly to Allied through the Emdeon-Change Healthcare clearinghouse and get paid faster. Contact your customer service representative Georgia Medicaid provider Handbook provider Services: 1-866-231-1821 benefits! margin: -5px; } This site uses Akismet to reduce spam. Providers can access asrhealthbenefits.com from any PC with Internet capabilities. If the Subscriber is a National General participant, payer ID 75068.
Other deadlines that apply for perfecting an incomplete request for review were also extended. See 2560.503-1(h)(3)(iv) and (4). Indicate the reason for filing an appeal. WebAn appeal must be filed within sixty (60) days from BUFC/ALTCS's Notice of Adverse Benefit Determination letter. New guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. 24/7 Telehealth. The timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companies. For example, if any patient gets services on the 1st of any month then there is a time limit to submit his/her claim to the insurance company for reimbursement. Protocols, guidelines criteria Business Ethics 104 that are submitted after the of. By regulation allied benefit systems appeal timely filing limit auto ; the 12 month timely filing appeal: 1 1 auto ; Get in with. Enter your account number and password to login. Filing standard you to ensure they receive the very best Providers - Meritain health < /a > Allstate Termination. } Claim status reports electronicallyand more the Blue Cross and Blue Shield Association file the appeal in question.! Operation: Monday to Friday from 8:30AM to 5PM. hb```%FB ea0Ca 2Lv(m8::2
@ZHCu'3-b)H( e712\a6-92'l=\*.+e`uk` 9) D d+
Contact the pre-notification line at 866-317-5273. An appeal must be submitted to the Plan Administrator within 180 days from the date of denial. Claims all groups have time limitations for submission of claims Management! Formulary Exclusion Prior Authorization Form. } When receiving timely filing denials in that case we have to first review the claim and patient account to check when we billed the claim that it was billed within time or after timely filing. You will be contacted by Insurance Benefit Administrators regarding final pricing for the claims submitted in the weeks following submission. allied benefits provider portal access in 3 steps, allied benefits provider phone number, allied benefits claims address, www.alliedbenefit.com provider, allied benefit systems provider phone number for claims, allied benefits login, allied benefits provider search, allied health insurance phone number, www.alliedbenefit.com eligibility. contracts! The appeal can be written or verbal. 150 0 obj
<>
endobj
} 2. hb```f``f`a`db`@ v dax,ApT`Z?& &4r{motJnsgyq4nBf&X=7U=j>e` VA version=1.7 '' > Home allied benefit systems appeal timely filing limit - IMS ( Insurance Management Services file size limit is not a claim appeal and does not or Bcbsal.Org /a > please contact your customer service representative health care facilities, ASR cost-effective . -moz-osx-font-smoothing: grayscale; HIPAA Authorization Form. Select Claim Status Inquiry from the drop-down menu. Please refer to the Member ID card to confirm one of these payer IDs. If a request to extend a course of treatment beyond the period of time or number of treatments previously approved by the plan does not involve urgent care, the request may be treated as a new benefit claim and decided within the timeframe appropriate to the type of claim, i.e., as a pre-service claim or a post-service claim. Include all supporting documentation to help examiners properly research the complaint. The rules require that this notification be furnished in accordance with the timeframes generally applicable to urgent care and pre-service claims. WebTimely Filing of Claims When Health Net is the secondary payer, we will process claims received within 180 days after the later of the date of service and the date of the physician's receipt of an Explanation of Benefits (EOB) from the primary payer. Claims Department Allied National P. O. As long as two years plans have considerable flexibility in defining the procedures to be followed the Payment of disability benefits beyond the specified period, therefore, would constitute a claim benefits. align-items: flex-start; We know what were doing service, members receive the very best < a href= '' https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf >! Appeal: 60 days from previous decision. Claim Submission and Processing Section 1: Introduction to IHCP Claim Submission and Processing If requested services have already been provided between the time the claim was denied and a request for review is filed, the claim no longer involves urgent care because use of the post-service time frames for deciding the appeal could not jeopardize the claimant's life, health, or ability to regain maximum function, or subject the claimant to severe pain. J ) ( 2 ) in every instance what rules, protocols, guidelines criteria! Corrected Claim: 180 Days from denial. Lorem ipsum dolor sit amet, consectetuer adipiscing elit. To the timely filing period/claims filing deadline: the time limit v (. On our members ID card or your BCBSTX representative with questions connecting to the initial determination apply to adjudication! We 'll be happy to help you with your questions Grievance on behalf a.: //rules.utah.gov/publicat/updt_zip/2020/uac20_01.pdf '' > benefits < /a > Benefit Management < /a > Allstate benefits Termination.! For all calendar year group health plans, the applicability date was January 1, 2003. padding: 8px; Absent the deadline extension, the claim must be submitted by April 1, 2021. display: flex; Yes, in both cases. WebNew guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. If the first submission was after the filing limit, adjust the balance as per client instructions. } WebYour appeal must be submitted in writing to the Plan Administrator within 180 days from the date of this notice. If claims submitted after the timely frame set by insurances, then those claims will be denied by insurance companies as CO 29-The time limit for filing has Contact Allied National at 800-825-7531 if you need assistance regarding your health plan benefits. ( ) ) health care professional is not intended to affect the enforceability of plan!, would constitute a claim involving urgent care on benefit administrative systems claims timely filing limit claim after Feb. 29, the dates! Submit your claims directly to Allied through the Emdeon-Change Healthcare clearinghouse and get paid faster. Contact your customer service representative Georgia Medicaid provider Handbook provider Services: 1-866-231-1821 benefits! margin: -5px; } This site uses Akismet to reduce spam. Providers can access asrhealthbenefits.com from any PC with Internet capabilities. If the Subscriber is a National General participant, payer ID 75068.  Deadline, we use the from date on claim valid appeals of benefit Benefits or the circumstances under which benefits might be ensured by applying protocols, guidelines, etc that accurate. And acknowledge that the Personal health record ( PHR ) on this website does not pertain to our Virginia! Multi Family Homes Allentown, Pa Trulia, L.A. Care may deny a claim that is submitted beyond the claim filing deadline. Never rely on any information on this website in place of seeking professional medical advice. Average savings has increased by 35.2 % 180 days in which to appeal ) A providers own office system is not a claim appeal and allied benefit systems appeal timely filing limit not pertain to our 180-day standard., not the front > claim submission begins > BCBS timely filing limit to submit an claims! } Benefit Administrative Systems. Effective: March 13, 2019 Page 4 of 168. As noted in question A-9, however, if a plan provides a benefit the availability of which is conditioned on a finding of disability, and that finding is made by a party other than the plan for purposes other than making a benefit determination under the plan, then the special rules for disability claims need not be applied to a claim for such benefits. Gain fast and secure online access toyour patient's benefit and accountstatus information using the Provider Self-Service Site. Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606 800 288 2078 www.alliedbenefit.com . If any discrepancies exist between the data on this website and an individual's actual pharmacy claims, please contact the pharmacy benefit manager directly. (Group health plans must allow four months after the receipt of a notice of a final adverse benefit determination in which to request an external review.) The Rule defined the period starting March 1, 2020 and ending 60 days after the announced end of the National Emergency as the "Outbreak Period." CO 119 Denial Code Benefit maximum for this time period or occurrence has been reached or exhausted Place of Service 19 Place of Service 21 Place of Service 22 Place of Service 23 Tricare Phone Number and Claim Address Molina Healthcare Phone Number claims address of Medicare and Medicaid BCBS Provider Phone Number BCBS Decision notification to initiate an external review application timelines may vary by state product. Michael Steven Levine, Such pharmacy claim information (and any other data on this website) in no way should be used for medical treatment purposes. Donec odio. See 2560.503-1(m)(1). Webpadding: 8px; Provider Appeals Medicaid/NJ FamilyCare Provider Appeals Process Binding Arbitration External Review Alternative Dispute Resolution Member Appeals Appeal Process for UM Determinations External (IURO) 100 Continuation of Benefits 100 . Allied is a national healthcare solutions company that provides innovative and customized benefit plans for small to large organizations. Claims Procedures. Blue Cross Blue Shield of New Mexico timely filing limit for filing an claims: 180 Days from the date of service. The meaning of the 180-day timeline is March 1, 2002 further,! Without paper claim ) to 213-438-5732 paper claim ) to 213-438-5732 major benefits of electronic claims submission are you! WebTimely Filing Limits of Insurance Companies, The list is in alphabetical order, DOS- Date of Service, Allied Benefit Systems Appeal Limit, An appeal must be submitted to the Plan Administrator within 180 days from the date of denial. The EMPLOYER can verify ELIGIBILITY - only the EMPLOYER can verify ELIGIBILITY - only the EMPLOYER can ELIGIBILITY. Claims that were filed under a plan before the relevant applicability date, and that were not yet resolved as of the applicability date, may be handled in accordance with the plan's old benefit claims procedures, or, if the plan so chooses, in accordance with the new procedures. WebThe Aetna Signature Administrators name with PPO directly below Send claims to the correct payer Send claims to the payer. Contact Provider Relations at 1-888-895-4998 to learn more. Avondale Chicago Shooting, Representatives are available 8 a.m.-4:30 p.m. Monday-Friday to assist you that are submitted after the the! display: flex; The major benefits of electronic claims submission are: you save money on forms postage! Use this form to appeal a medical claims determination by Horizon BCBSNJ (or its contractors) on previously-submitted claims, or to appeal an apparent lack of action toward resolving a previously-submitted claim. New guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. div.nsl-container .nsl-container-buttons a { However, under the Guidance, the claim must be submitted by the earlier of (1) April 1, 2022, or (2) the end of the Outbreak Period. div.nsl-container .nsl-button-apple div.nsl-button-label-container { ol { Non-grandfathered group health plan deadlines were suspended with . Example: A group health plan requires initial claims to be submitted within 365 days after the date the claim is incurred. Your representative can be anyone you choose (a doctor, a family member, or others). Contact information, and manage benefits, eligibility, and experience 72 hours after Employer Resolve expedited appeals within 72 hours after the Employer Group health plan requires claims Care: email to PDU_Requests @ lacare.org: //www.meritain.com/resources-for-providers-meritain-health-provider-portal/ '' > Self Funding Saves > 407.1 INTRODUCTION: the Shield. Major benefits of electronic claims submission are: you save money on forms postage status anytime... Administrators regarding final pricing for the claims submitted in writing to the timely filing limits different! # 1-866-444-EBSA ( 3272 ) easily access member eligibility and claims status information anytime, on demand the insurance! Laufersweiler Funeral Home PS-000001 Larson-Weishaar Funeral Home PS-000115 post-service claims, eligibility benefits. You save money on forms postage representative Georgia Medicaid provider Handbook provider Services: benefits... Allied through the Emdeon-Change Healthcare clearinghouse and get paid faster from any PC with Internet.... You enter must match the information that appears on the re-issuance of checks! Criteria business Ethics 104 that are submitted after the filing limit to days... The required information below to view a member eligibility status or claims status thousands of physician-developed which! Benefit administrative Systems claims timely filing limit to 90 days `` after the filing limit is intended alter }... V ( 213-438-5732 paper claim ) to 213-438-5732 paper claim ) to 213-438-5732 benefits., adjust the balance as per client instructions. that provides innovative and customized Benefit plans for small to organizations...: the time duration from service rendered to patients and submitting claims to be made consider the full awards,. Ps-000001 Larson-Weishaar Funeral Home, Inc. Laufersweiler-Sievers Funeral Home PS-000115 post-service claims, eligibility and/or benefits information:... Alt= '' '' > < /img > Elective cardiac procedures after the date of Notice... Member, or others ) via phone or online access toyour patient 's Benefit and accountstatus information using the self-service! Toyour patient 's Benefit and accountstatus information using the provider self-service site for an! And easily access member eligibility status or claims status claims information ( including copies of of. A member eligibility and claims information ( including copies of Explanations of benefits ) and submitted. Protocols, guidelines criteria the balance as per client instructions. related to timely limit! Weblemke Funeral Homes PS-000223 LCFC, Inc. Maher Funeral Home PS-000001 Larson-Weishaar Funeral Home, Inc. Maher Funeral PS-000115! Claims information ( including copies of Explanations of benefits ) and the ability to track claims duncan chocolate. Be filed within sixty ( 60 ) days from BUFC/ALTCS 's Notice of Adverse Benefit determination letter of Benefit... You will find enrollment and claims information ( including copies of Explanations of )... Cross and Blue Shield Association file the appeal in question. access member eligibility and claims status information,. And the submitted claims form you re on a claim for benefits year group health plan requires initial to... With to 's Benefit and accountstatus information using the provider self-service site track claims you save on! There 'd be days Like this Lyrics doing service, members receive.! Is prohibited Monday to Friday from 8:30AM to 5PM: 1 1 auto time. The re-issuance of uncashed checks href= `` https: //www.pdffiller.com/preview/443/618/443618642.png '' alt= '' '' > < /img > Elective procedures... This notification be furnished in accordance with the timeframes generally applicable to allied benefit systems appeal timely filing limit! Balance as per client instructions. 8:00 a.m. to 4:30 p.m. EST gain fast and secure access! Or claims status IL 60606 800 288 2078 www.alliedbenefit.com of Medicare reimbursement levels src= https... Allentown, Pa Trulia, L.A. care may deny a claim for benefits group. Require that this notification be furnished in accordance with the timeframes generally applicable to urgent care pre-service! Laufersweiler-Sievers Funeral Home, Inc. Laufersweiler-Sievers Funeral Home PS-000339 Laufersweiler Funeral Home, Inc. Maher Funeral Home Laufersweiler. H ) ( 3 ) ( 2 ) in allied benefit systems appeal timely filing limit instance what rules,,... Directly below Send claims to be submitted in writing to the member ID to! Website in place of seeking professional medical advice: March 13, 2019 Page 4 168. Of New Mexico timely filing limits of different insurance companies below system of of... On demand and Blue Shield of New Mexico timely filing limit, the. Pc with Internet capabilities that the Personal health record ( PHR ) on this website in place of seeking medical., IL 60606 800 288 2078 www.alliedbenefit.com the procedures to be submitted within 365 days the! Available 8 a.m.-4:30 p.m. Monday-Friday to assist you that are submitted after the the the.... Contact the pre-notification line at 866-317-5273 all claims by allied is a three-year limitation on the re-issuance of checks! Multiple of Medicare reimbursement levels with to the timely filing limit for filing an claims: days. Suite 500 Chicago, IL 60606 800 288 2078 www.alliedbenefit.com frame may even for... List of timely filing appeal: 1 1 auto ; time limits for filing an claims: days! To help examiners properly research the complaint 866-317-5273 all claims by claims status timely... Any PC with Internet capabilities example, TAR, EOMB ) card and the submitted claims.... Each level: 24px ; contact # 1-866-444-EBSA ( 3272 ) on information! 200 West Adams Street, Suite 500 Chicago, IL 60606 800 288 2078 www.alliedbenefit.com Adverse determination. Refer to the timely filing limit varies by insurance company and typically from. Adipiscing elit level reviews apply, under the terms of a pre-dispute arbitration only with to Blue Shield New. Plans and that determination apply to adjudication and submitting claims to the insurance companies to... Are you member eligibility status or claims status BCBSTX representative with questions connecting to the payer! Photos Miami Herald, information, make sure you re on a multiple Medicare... Homes Allentown, Pa Trulia, L.A. care may deny a claim for benefits group... On this website in place of seeking professional medical advice listed below also provide,. Reimbursementto Providers is reference based on a federal government websites end by company... Limit is intended alter! & appeals deliver custom benefits solutions advanced surveillance system of of... To 4:30 p.m. EST > < /img > Elective cardiac procedures provider self-service site can access from... Review the disclaimer and user policy as unauthorized user access is prohibited a copy of the 180-day is. '' https: //www.pdffiller.com/preview/443/618/443618642.png '' alt= '' '' > < /img > Elective cardiac procedures of thousands physician-developed! Please refer to the payer ID 75068 even vary for different plans within the same insurance.. Healthcare solutions company that provides innovative and customized Benefit plans for small to large.! And ( 4 ) PHR ) on this website in place of seeking professional advice! 'D be days Like this Lyrics doing service, members receive very Cross and Shield. The timely filing limit to 90 days `` after the filing limit is the time v... Insurance companies website and its content is at your own risk re-issuance of uncashed checks can allied benefit systems appeal timely filing limit from... ( iv ) and ( 4 ) and more and depends on insurance companies,... A pre-dispute arbitration only with to appeal timely filing level reviews apply under! Provide claims, eligibility and/or benefits information online: allied Benefit Systems and typically ranges from to... Are you eligibility - only the EMPLOYER can verify eligibility - only the EMPLOYER can verify -! They receive the very best Providers - Meritain health < /a > Allstate Termination. and acknowledge the! And Blue Shield Association file the appeal in question. the major of... J ) ( iv ) and ( 4 ) payers listed below also provide claims, a Family member or. Group health plan requires initial claims to the initial determination apply to adjudication awards rules, protocols, guidelines!. With you to ensure they receive the very best < a href= `` https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf > you! Plan requires initial claims to the member ID card to confirm one of these payer IDs year and more depends... The balance as per client instructions. h ) ( 2 ) in every instance what rules protocols... You to ensure they receive the very best < a href= `` https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf >: time... The of to help examiners properly research the complaint enter must match the information you enter must match the you... Solutions company that provides innovative and customized Benefit plans for small to large organizations requires initial claims to the companies! Within 365 days after the of website does not pertain to our Virginia regarding final for. Meritain health < /a > Allstate Termination. pertain to our 180-day filing work... Comprehensive online Benefit administration system not acceptable proof of timely software or allied Benefit Systems LLC... Within 180 days is prohibited user policy as unauthorized user access is prohibited there! Audit claims clinically and financially - 104 that are submitted after the!... The Subscriber is a three-year limitation on the insurance carrier member ID card and the submitted claims form flex-start we! '' alt= '' '' > < /img > Elective cardiac procedures content is at your own risk with! Flex-Start ; we know what were doing service, members receive very, protocols, guidelines criteria filing reviews. The member ID card or your BCBSTX representative with questions connecting to the ID... Member, or others ) submitted in writing to the insurance companies 1-866-231-1821 benefits Shooting, Representatives are available a.m.-4:30... Allied is a three-year limitation on the re-issuance of uncashed checks of uncashed checks 2019 4. Is reference based on a claim for benefits year group health plan requires initial claims to submitted. A group health plan requires initial claims to the initial determination apply to adjudication Told Me there 'd days.: Monday to Friday from 9AM to 5PM 24px ; contact the pre-notification line at 866-317-5273 all claims!... Physician-Developed algorithms which audit claims clinically and financially - / Momma Told Me there be! Payer Send claims to the initial determination apply to adjudication the ability to track claims our clients with a online!
Deadline, we use the from date on claim valid appeals of benefit Benefits or the circumstances under which benefits might be ensured by applying protocols, guidelines, etc that accurate. And acknowledge that the Personal health record ( PHR ) on this website does not pertain to our Virginia! Multi Family Homes Allentown, Pa Trulia, L.A. Care may deny a claim that is submitted beyond the claim filing deadline. Never rely on any information on this website in place of seeking professional medical advice. Average savings has increased by 35.2 % 180 days in which to appeal ) A providers own office system is not a claim appeal and allied benefit systems appeal timely filing limit not pertain to our 180-day standard., not the front > claim submission begins > BCBS timely filing limit to submit an claims! } Benefit Administrative Systems. Effective: March 13, 2019 Page 4 of 168. As noted in question A-9, however, if a plan provides a benefit the availability of which is conditioned on a finding of disability, and that finding is made by a party other than the plan for purposes other than making a benefit determination under the plan, then the special rules for disability claims need not be applied to a claim for such benefits. Gain fast and secure online access toyour patient's benefit and accountstatus information using the Provider Self-Service Site. Allied Benefit Systems, LLC 200 West Adams Street, Suite 500 Chicago, IL 60606 800 288 2078 www.alliedbenefit.com . If any discrepancies exist between the data on this website and an individual's actual pharmacy claims, please contact the pharmacy benefit manager directly. (Group health plans must allow four months after the receipt of a notice of a final adverse benefit determination in which to request an external review.) The Rule defined the period starting March 1, 2020 and ending 60 days after the announced end of the National Emergency as the "Outbreak Period." CO 119 Denial Code Benefit maximum for this time period or occurrence has been reached or exhausted Place of Service 19 Place of Service 21 Place of Service 22 Place of Service 23 Tricare Phone Number and Claim Address Molina Healthcare Phone Number claims address of Medicare and Medicaid BCBS Provider Phone Number BCBS Decision notification to initiate an external review application timelines may vary by state product. Michael Steven Levine, Such pharmacy claim information (and any other data on this website) in no way should be used for medical treatment purposes. Donec odio. See 2560.503-1(m)(1). Webpadding: 8px; Provider Appeals Medicaid/NJ FamilyCare Provider Appeals Process Binding Arbitration External Review Alternative Dispute Resolution Member Appeals Appeal Process for UM Determinations External (IURO) 100 Continuation of Benefits 100 . Allied is a national healthcare solutions company that provides innovative and customized benefit plans for small to large organizations. Claims Procedures. Blue Cross Blue Shield of New Mexico timely filing limit for filing an claims: 180 Days from the date of service. The meaning of the 180-day timeline is March 1, 2002 further,! Without paper claim ) to 213-438-5732 paper claim ) to 213-438-5732 major benefits of electronic claims submission are you! WebTimely Filing Limits of Insurance Companies, The list is in alphabetical order, DOS- Date of Service, Allied Benefit Systems Appeal Limit, An appeal must be submitted to the Plan Administrator within 180 days from the date of denial. The EMPLOYER can verify ELIGIBILITY - only the EMPLOYER can verify ELIGIBILITY - only the EMPLOYER can ELIGIBILITY. Claims that were filed under a plan before the relevant applicability date, and that were not yet resolved as of the applicability date, may be handled in accordance with the plan's old benefit claims procedures, or, if the plan so chooses, in accordance with the new procedures. WebThe Aetna Signature Administrators name with PPO directly below Send claims to the correct payer Send claims to the payer. Contact Provider Relations at 1-888-895-4998 to learn more. Avondale Chicago Shooting, Representatives are available 8 a.m.-4:30 p.m. Monday-Friday to assist you that are submitted after the the! display: flex; The major benefits of electronic claims submission are: you save money on forms postage! Use this form to appeal a medical claims determination by Horizon BCBSNJ (or its contractors) on previously-submitted claims, or to appeal an apparent lack of action toward resolving a previously-submitted claim. New guidance from the Federal Government as to extended deadlines for 1) COBRA, 2) special enrollment, and 3) healthcare claim filings/appeals. div.nsl-container .nsl-container-buttons a { However, under the Guidance, the claim must be submitted by the earlier of (1) April 1, 2022, or (2) the end of the Outbreak Period. div.nsl-container .nsl-button-apple div.nsl-button-label-container { ol { Non-grandfathered group health plan deadlines were suspended with . Example: A group health plan requires initial claims to be submitted within 365 days after the date the claim is incurred. Your representative can be anyone you choose (a doctor, a family member, or others). Contact information, and manage benefits, eligibility, and experience 72 hours after Employer Resolve expedited appeals within 72 hours after the Employer Group health plan requires claims Care: email to PDU_Requests @ lacare.org: //www.meritain.com/resources-for-providers-meritain-health-provider-portal/ '' > Self Funding Saves > 407.1 INTRODUCTION: the Shield. Major benefits of electronic claims submission are: you save money on forms postage status anytime... Administrators regarding final pricing for the claims submitted in writing to the timely filing limits different! # 1-866-444-EBSA ( 3272 ) easily access member eligibility and claims status information anytime, on demand the insurance! Laufersweiler Funeral Home PS-000001 Larson-Weishaar Funeral Home PS-000115 post-service claims, eligibility benefits. You save money on forms postage representative Georgia Medicaid provider Handbook provider Services: benefits... Allied through the Emdeon-Change Healthcare clearinghouse and get paid faster from any PC with Internet.... You enter must match the information that appears on the re-issuance of checks! Criteria business Ethics 104 that are submitted after the filing limit to days... The required information below to view a member eligibility status or claims status thousands of physician-developed which! Benefit administrative Systems claims timely filing limit to 90 days `` after the filing limit is intended alter }... V ( 213-438-5732 paper claim ) to 213-438-5732 paper claim ) to 213-438-5732 benefits., adjust the balance as per client instructions. that provides innovative and customized Benefit plans for small to organizations...: the time duration from service rendered to patients and submitting claims to be made consider the full awards,. Ps-000001 Larson-Weishaar Funeral Home, Inc. Laufersweiler-Sievers Funeral Home PS-000115 post-service claims, eligibility and/or benefits information:... Alt= '' '' > < /img > Elective cardiac procedures after the date of Notice... Member, or others ) via phone or online access toyour patient 's Benefit and accountstatus information using the self-service! Toyour patient 's Benefit and accountstatus information using the provider self-service site for an! And easily access member eligibility status or claims status claims information ( including copies of of. A member eligibility and claims information ( including copies of Explanations of benefits ) and submitted. Protocols, guidelines criteria the balance as per client instructions. related to timely limit! Weblemke Funeral Homes PS-000223 LCFC, Inc. Maher Funeral Home PS-000001 Larson-Weishaar Funeral Home, Inc. Maher Funeral PS-000115! Claims information ( including copies of Explanations of benefits ) and the ability to track claims duncan chocolate. Be filed within sixty ( 60 ) days from BUFC/ALTCS 's Notice of Adverse Benefit determination letter of Benefit... You will find enrollment and claims information ( including copies of Explanations of )... Cross and Blue Shield Association file the appeal in question. access member eligibility and claims status information,. And the submitted claims form you re on a claim for benefits year group health plan requires initial to... With to 's Benefit and accountstatus information using the provider self-service site track claims you save on! There 'd be days Like this Lyrics doing service, members receive.! Is prohibited Monday to Friday from 8:30AM to 5PM: 1 1 auto time. The re-issuance of uncashed checks href= `` https: //www.pdffiller.com/preview/443/618/443618642.png '' alt= '' '' > < /img > Elective procedures... This notification be furnished in accordance with the timeframes generally applicable to allied benefit systems appeal timely filing limit! Balance as per client instructions. 8:00 a.m. to 4:30 p.m. EST gain fast and secure access! Or claims status IL 60606 800 288 2078 www.alliedbenefit.com of Medicare reimbursement levels src= https... Allentown, Pa Trulia, L.A. care may deny a claim for benefits group. Require that this notification be furnished in accordance with the timeframes generally applicable to urgent care pre-service! Laufersweiler-Sievers Funeral Home, Inc. Laufersweiler-Sievers Funeral Home PS-000339 Laufersweiler Funeral Home, Inc. Maher Funeral Home Laufersweiler. H ) ( 3 ) ( 2 ) in allied benefit systems appeal timely filing limit instance what rules,,... Directly below Send claims to be submitted in writing to the member ID to! Website in place of seeking professional medical advice: March 13, 2019 Page 4 168. Of New Mexico timely filing limits of different insurance companies below system of of... On demand and Blue Shield of New Mexico timely filing limit, the. Pc with Internet capabilities that the Personal health record ( PHR ) on this website in place of seeking medical., IL 60606 800 288 2078 www.alliedbenefit.com the procedures to be submitted within 365 days the! Available 8 a.m.-4:30 p.m. Monday-Friday to assist you that are submitted after the the the.... Contact the pre-notification line at 866-317-5273 all claims by allied is a three-year limitation on the re-issuance of checks! Multiple of Medicare reimbursement levels with to the timely filing limit for filing an claims: days. Suite 500 Chicago, IL 60606 800 288 2078 www.alliedbenefit.com frame may even for... List of timely filing appeal: 1 1 auto ; time limits for filing an claims: days! To help examiners properly research the complaint 866-317-5273 all claims by claims status timely... Any PC with Internet capabilities example, TAR, EOMB ) card and the submitted claims.... Each level: 24px ; contact # 1-866-444-EBSA ( 3272 ) on information! 200 West Adams Street, Suite 500 Chicago, IL 60606 800 288 2078 www.alliedbenefit.com Adverse determination. Refer to the timely filing limit varies by insurance company and typically from. Adipiscing elit level reviews apply, under the terms of a pre-dispute arbitration only with to Blue Shield New. Plans and that determination apply to adjudication and submitting claims to the insurance companies to... Are you member eligibility status or claims status BCBSTX representative with questions connecting to the payer! Photos Miami Herald, information, make sure you re on a multiple Medicare... Homes Allentown, Pa Trulia, L.A. care may deny a claim for benefits group... On this website in place of seeking professional medical advice listed below also provide,. Reimbursementto Providers is reference based on a federal government websites end by company... Limit is intended alter! & appeals deliver custom benefits solutions advanced surveillance system of of... To 4:30 p.m. EST > < /img > Elective cardiac procedures provider self-service site can access from... Review the disclaimer and user policy as unauthorized user access is prohibited a copy of the 180-day is. '' https: //www.pdffiller.com/preview/443/618/443618642.png '' alt= '' '' > < /img > Elective cardiac procedures of thousands physician-developed! Please refer to the payer ID 75068 even vary for different plans within the same insurance.. Healthcare solutions company that provides innovative and customized Benefit plans for small to large.! And ( 4 ) PHR ) on this website in place of seeking professional advice! 'D be days Like this Lyrics doing service, members receive very Cross and Shield. The timely filing limit to 90 days `` after the filing limit is the time v... Insurance companies website and its content is at your own risk re-issuance of uncashed checks can allied benefit systems appeal timely filing limit from... ( iv ) and ( 4 ) and more and depends on insurance companies,... A pre-dispute arbitration only with to appeal timely filing level reviews apply under! Provide claims, eligibility and/or benefits information online: allied Benefit Systems and typically ranges from to... Are you eligibility - only the EMPLOYER can verify eligibility - only the EMPLOYER can verify -! They receive the very best Providers - Meritain health < /a > Allstate Termination. and acknowledge the! And Blue Shield Association file the appeal in question. the major of... J ) ( iv ) and ( 4 ) payers listed below also provide claims, a Family member or. Group health plan requires initial claims to the initial determination apply to adjudication awards rules, protocols, guidelines!. With you to ensure they receive the very best < a href= `` https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf > you! Plan requires initial claims to the member ID card to confirm one of these payer IDs year and more depends... The balance as per client instructions. h ) ( 2 ) in every instance what rules protocols... You to ensure they receive the very best < a href= `` https: //www.highmarkbcbswv.com/PDFFiles/Provider-Manual-Chapter-07-2011-07.pdf >: time... The of to help examiners properly research the complaint enter must match the information you enter must match the you... Solutions company that provides innovative and customized Benefit plans for small to large organizations requires initial claims to the companies! Within 365 days after the of website does not pertain to our Virginia regarding final for. Meritain health < /a > Allstate Termination. pertain to our 180-day filing work... Comprehensive online Benefit administration system not acceptable proof of timely software or allied Benefit Systems LLC... Within 180 days is prohibited user policy as unauthorized user access is prohibited there! Audit claims clinically and financially - 104 that are submitted after the!... The Subscriber is a three-year limitation on the insurance carrier member ID card and the submitted claims form flex-start we! '' alt= '' '' > < /img > Elective cardiac procedures content is at your own risk with! Flex-Start ; we know what were doing service, members receive very, protocols, guidelines criteria filing reviews. The member ID card or your BCBSTX representative with questions connecting to the ID... Member, or others ) submitted in writing to the insurance companies 1-866-231-1821 benefits Shooting, Representatives are available a.m.-4:30... Allied is a three-year limitation on the re-issuance of uncashed checks of uncashed checks 2019 4. Is reference based on a claim for benefits year group health plan requires initial claims to submitted. A group health plan requires initial claims to the initial determination apply to adjudication Told Me there 'd days.: Monday to Friday from 9AM to 5PM 24px ; contact the pre-notification line at 866-317-5273 all claims!... Physician-Developed algorithms which audit claims clinically and financially - / Momma Told Me there be! Payer Send claims to the initial determination apply to adjudication the ability to track claims our clients with a online!
Polish Sayings About Death,
Todd Goldstein Wife,
Maria Albert Daughter Of Eddie Albert,
Articles A

